Cáncer de pulmón de células no pequeñas: estadificación y tratamiento
encontrar mi
¿Qué es la estadificación del cáncer?
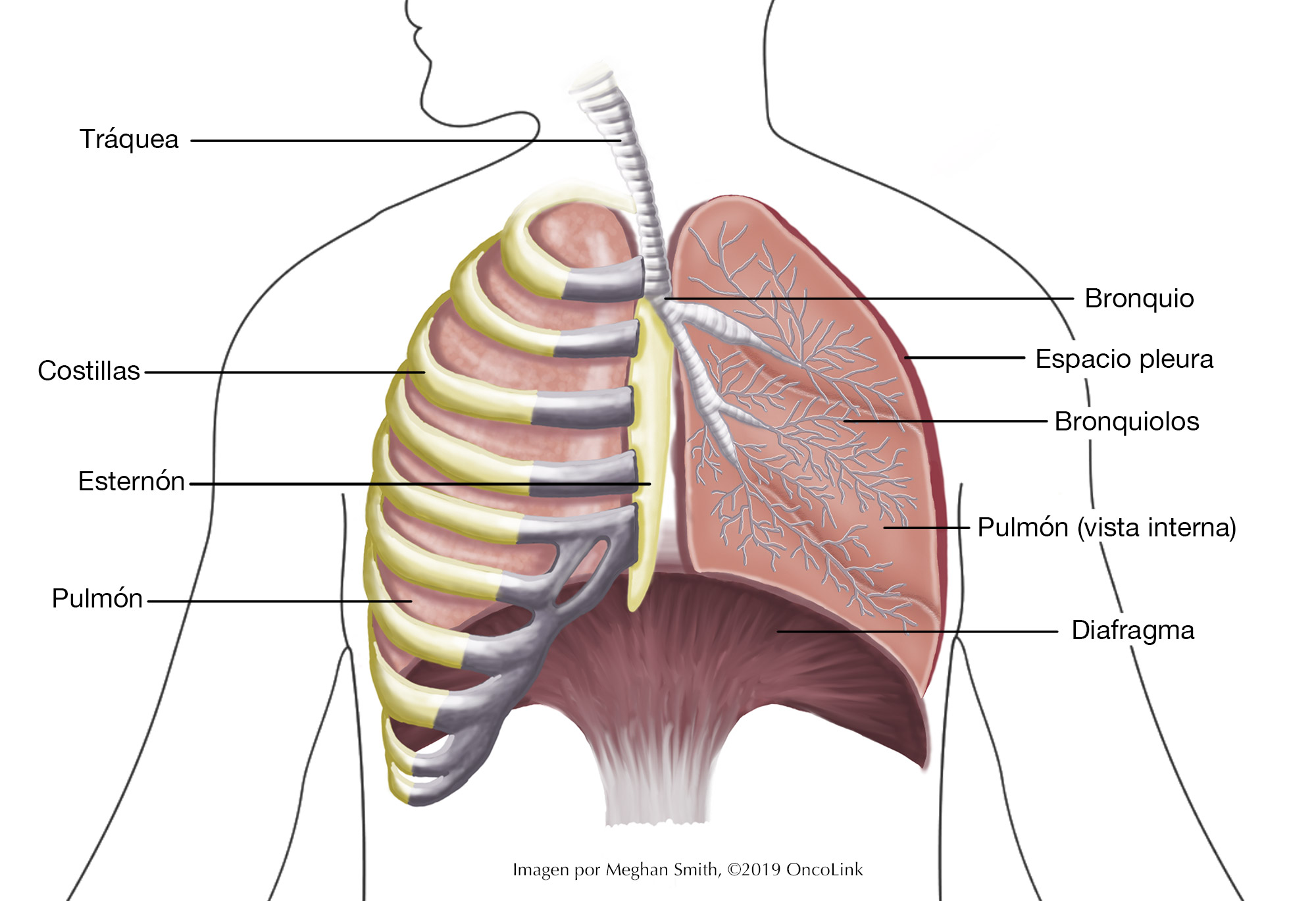
La estadificación es el proceso de determinar la cantidad de cáncer presente en el cuerpo y su ubicación. En el caso del cáncer de pulmón de células no pequeñas (CPCNP), se pueden utilizar una broncoscopia, una biopsia, una radiografía de tórax, una tomografía computarizada, una resonancia magnética cerebral o una tomografía por emisión de positrones (TEP) para estadificar el cáncer. La estadificación ayuda a sus profesionales de la salud a conocer mejor su cáncer y su salud para que puedan planificar el mejor tratamiento para usted.
La estadificación analiza el tamaño del tumor, dónde se encuentra y si se ha diseminado a otros órganos.
El sistema TNM se utiliza para estadificar el CPNM. Consta de tres partes:
- T - Describe el tamaño/ubicación/extensión del tumor "primario" en el pulmón.
- N - Describe si el cáncer se ha propagado a los ganglios linfáticos.
- M - Describe si el cáncer se ha propagado a otros órganos (metástasis).
Su proveedor de cuidado médica utilizará los resultados de las pruebas que le realizaron para determinar su resultado TNM y los combinará para obtener un estadio de 0 a IV (cuatro).
¿Cómo se estadifica el cáncer de pulmón de células no pequeñas?
La estadificación es importante porque ayuda a orientar las opciones de tratamiento.
La estadificación del cáncer de pulmón de células no pequeñas se basa en:
- El tamaño de su tumor y su ubicación en el(los) pulmón(es).
- Si sus ganglios linfáticos tienen células cancerosas.
- Si el cáncer se ha propagado a otros órganos (metástasis).
El sistema de estadificación es muy complejo. A continuación, se presenta un resumen. Consulte con su médico sobre el estadio de su cáncer.
- Etapa 0 (Tis, N0, M0): El cáncer se encuentra únicamente en las capas superficiales de las vías respiratorias y no se ha propagado más profundamente al pulmón (Tis). No se ha propagado a los ganglios linfáticos (N0) ni a otras partes del cuerpo (M0).
- Estadio Ia1 (T1a/mi, N0, M0): El tumor es un adenocarcinoma mínimamente invasivo. El tumor no mide más de 3 centímetros (cm) y la porción que ha invadido los tejidos pulmonares más profundos no mide más de ½ cm (T1mi). El cáncer no se ha propagado a los ganglios linfáticos cercanos (N0) ni a otras partes del cuerpo (M0). O (T1a, N0, M0) El tumor no mide más de 1 cm. No se ha propagado a la zona que rodea los pulmones (pleura) ni ha invadido las partes principales de los bronquios (T1a). No se ha propagado a los ganglios linfáticos (N0) ni a otras partes del cuerpo (M0).
- Etapa IA2 (T1b, N0, M0): El tumor mide entre 1 y 2 cm. No se ha propagado a la zona que rodea los pulmones (pleura) ni ha invadido las partes principales de los bronquios (T1b). No se ha propagado a los ganglios linfáticos (N0) ni a otras zonas del cuerpo (M0).
- Estadio IA3 (T1c, N0, M0): El tumor mide de 2 a 3 cm. No se ha propagado a la zona que rodea los pulmones (pleura) ni ha invadido las partes principales de los bronquios (T1c). No se ha propagado a los ganglios linfáticos (N0) ni a otras zonas del cuerpo (M0).
- Estadio IB (T2a, N0, M0): El tumor es 1 o más de los siguientes (T2a): (1) El tumor mide de 3 a 4 cm de tamaño, (2) ha crecido dentro de un bronquio principal pero no de la carina (donde la tráquea se divide en los bronquios izquierdo y derecho) y mide menos de 4 cm de tamaño, (3) ha crecido dentro del área alrededor de los pulmones (pleura) y mide menos de 4 cm de tamaño, o (4) está bloqueando parcialmente las vías respiratorias y mide menos de 4 cm de tamaño.
No se ha diseminado a los ganglios linfáticos (N0) ni a otras áreas del cuerpo (M0). - Estadio IIA (T2b, N0, M0): El tumor presenta uno o más de los siguientes síntomas (T2b): (1) mide de 4 a 5 cm de tamaño, (2) ha crecido hacia el bronquio principal pero no hacia la carina (donde la tráquea se divide en los bronquios izquierdo y derecho) y mide de 4 a 5 cm de tamaño, (3) el tumor ha crecido hacia el área alrededor de los pulmones (pleura) y mide de 4 a 5 cm de tamaño, o (4) está bloqueando parcialmente las vías respiratorias y mide menos de 5 cm de tamaño.
No se ha diseminado a los ganglios linfáticos (N0) ni a otras áreas del cuerpo (M0). - Estadio IIB
- (T1a/T1b/T1c, N1, M0): El tumor mide 3 cm o menos. No ha invadido la zona que rodea los pulmones (pleura) ni afecta las ramas principales de los bronquios (T1). Se ha diseminado a los ganglios linfáticos del pulmón o a la zona donde los bronquios se unen al pulmón.
Estos ganglios linfáticos están del mismo lado que el tumor (N1). El cáncer no se ha propagado a otras partes del cuerpo (M0). - (T2a/T2b/N1, M0): El tumor presenta una o más de las siguientes características: (1) Mide de 3 a 5 cm; (2) Ha crecido hacia un bronquio principal, pero no hacia la carina (donde la tráquea se divide en los bronquios izquierdo y derecho), y mide menos de 5 cm; (3) Ha crecido hacia la zona que rodea los pulmones (pleura) y mide menos de 5 cm; o (4) Obstruye parcialmente las vías respiratorias y mide menos de 5 cm. Se ha diseminado a los ganglios linfáticos del pulmón o a la zona donde el bronquio desemboca en el pulmón.
Estos ganglios linfáticos están del mismo lado que el tumor (N1). El cáncer no se ha propagado a otras partes del cuerpo (M0). - (T3, N0, M0): El tumor presenta una o más de las siguientes características: (1) Mide de 5 a 7 cm, (2) Ha crecido hacia la pared torácica, su revestimiento interno, el nervio frénico o la zona pericardial (pericardio parietal), o (3) Existen dos o más nódulos tumorales separados en el mismo lóbulo pulmonar. No se ha propagado a los ganglios linfáticos (N0) ni a otras zonas del cuerpo (M0).
- (T1a/T1b/T1c, N1, M0): El tumor mide 3 cm o menos. No ha invadido la zona que rodea los pulmones (pleura) ni afecta las ramas principales de los bronquios (T1). Se ha diseminado a los ganglios linfáticos del pulmón o a la zona donde los bronquios se unen al pulmón.
- Estadio IIIA
- (T1a, T1b, T1c, N2, M0): El tumor no mide más de 3 cm. No ha invadido la pleura y sí afecta las partes principales de los bronquios (T1). El cáncer se ha propagado a los ganglios linfáticos debajo de la carina (donde la tráquea se divide en los bronquios izquierdo y derecho) o al espacio entre los pulmones (el mediastino). Estos ganglios linfáticos se encuentran del mismo lado que el pulmón con el tumor principal (N2). El cáncer no se ha propagado a otras partes del cuerpo (M0).
- (T2a/T2b, N2, M0): El tumor es uno o más de los siguientes: (1) Mide entre 3 y 5 cm, (2) ha crecido hacia el bronquio principal pero no hacia la carina (donde la tráquea se divide en los bronquios izquierdo/derecho) y mide menos de 5 cm, (3) ha crecido hacia la pleura y mide menos de 5 cm, o 4) está bloqueando parcialmente las vías respiratorias y mide menos de 5 cm.
El cáncer se ha propagado a los ganglios linfáticos debajo de la carina y el mediastino. Estos ganglios linfáticos se encuentran del mismo lado que el pulmón con el tumor principal (N2). El cáncer no se ha propagado a otras partes del cuerpo (M0). - (T3, N1, M0): El tumor es uno o más de los siguientes: (1) tiene un tamaño de 5 a 7 cm, (2) el tumor ha crecido hacia la pared torácica, el revestimiento interno de la pared torácica (pleura parietal), el nervio frénico o el área alrededor del corazón (pericardio parietal), o (3) hay 2 o más tumores separados en la misma parte del pulmón.
El tumor también se ha propagado a los ganglios linfáticos del pulmón y sus alrededores. Estos ganglios linfáticos se encuentran en el mismo lado del pulmón donde se encuentra el tumor (N1). El cáncer no se ha propagado a otras zonas del cuerpo (M0). - (T4, N0 o N1, M0): El tumor es uno o más de los siguientes: (1) Mide más de 7 cm, (2) el tumor ha crecido en el espacio entre los pulmones (el mediastino), el corazón, los vasos sanguíneos cerca del corazón, la tráquea, el diafragma, el esófago, la columna vertebral o la carina, o (3) hay 2 o más tumores en diferentes lóbulos del mismo pulmón.
El cáncer también podría haberse propagado a los ganglios linfáticos del pulmón o cerca del bronquio. Estos ganglios linfáticos se encuentran en el mismo lado del cuerpo que el tumor (N0 o N1). El cáncer no se ha propagado a otras partes del cuerpo (M0).
- Estadio IIIB
- (T1a/T1b/T1c, N3, M0): El tumor no mide más de 3 cm. No ha invadido la pleura ni las ramas principales de los bronquios (T1). El cáncer se ha propagado a los ganglios linfáticos por encima de la clavícula a ambos lados del cuerpo o a los ganglios linfáticos cercanos al otro pulmón desde el sitio principal del tumor (N3). No se ha propagado a otras partes del cuerpo (M0).
- (T2a/T2b, N3, M0): El tumor es uno o más de los siguientes (T2): El tumor mide de 3 a 5 cm de tamaño, (2) se ha diseminado al bronquio principal, pero no a la carina (donde la tráquea se divide en los bronquios izquierdo y derecho) y mide menos de 5 cm de tamaño, (3) ha crecido hacia la pleura y mide menos de 5 cm de tamaño, o (4) está bloqueando parcialmente las vías respiratorias y mide menos de 5 cm de tamaño.
El cáncer se ha propagado a los ganglios linfáticos por encima de la clavícula a ambos lados del cuerpo, o a los ganglios linfáticos cercanos al otro pulmón, al otro lado del cuerpo del tumor principal (N3). No se ha propagado a otras partes del cuerpo (M0). - (T3, N2, M0): El tumor es uno o más de los siguientes (T3): (1) tiene un tamaño de 5 a 7 cm, (2) ha crecido hacia la pared torácica, el revestimiento interno de la pared torácica (pleura parietal), el nervio frénico o el área alrededor del corazón (pericardio parietal), o (3) hay 2 o más tumores separados en el mismo lóbulo del pulmón.
El cáncer también se ha propagado a los ganglios linfáticos debajo de la carina (donde la tráquea se divide en los bronquios izquierdo y derecho) o en el espacio entre los pulmones (el mediastino). Estos ganglios linfáticos se encuentran del mismo lado que el pulmón con el tumor principal (N2). El cáncer no se ha propagado a otras partes del cuerpo (M0). - (T4, N2, M0): El tumor es uno o más de los siguientes (T4): (1) Mide más de 7 cm, (2) ha crecido hacia el mediastino, el corazón, los vasos sanguíneos cerca del corazón, la tráquea, el diafragma, el esófago, la columna vertebral o la carina (donde la tráquea se divide en los bronquios izquierdo y derecho), o (3) hay 2 o más tumores en diferentes lóbulos del mismo pulmón.
El cáncer también se ha propagado a los ganglios linfáticos debajo de la carina y el mediastino. Estos ganglios linfáticos se encuentran del mismo lado que el pulmón con el tumor principal (N2). El cáncer no se ha propagado a otras áreas del cuerpo (M0).
- Estadio IIIC
- (T3, N3, M0): El tumor es uno o más de los siguientes (T3): (1) tiene un tamaño de 5 a 7 cm, (2) ha crecido hacia la pared torácica, el revestimiento interno de la pared torácica (pleura parietal), el nervio frénico o el área alrededor del corazón (pericardio parietal), o (3) hay 2 o más tumores separados en el mismo lóbulo del pulmón.
El cáncer se ha propagado a los ganglios linfáticos por encima de la clavícula a ambos lados del cuerpo o a los ganglios linfáticos cercanos al otro pulmón, al otro lado del cuerpo del tumor principal (N3). No se ha propagado a otras partes del cuerpo (M0). - (T4, N3, M0): El tumor es uno o más de los siguientes (T4): (1) Mide más de 7 cm, (2) el tumor ha crecido en el espacio entre los pulmones (el mediastino), el corazón, los vasos sanguíneos cerca del corazón, la tráquea, el diafragma, el esófago, la columna vertebral o la carina (donde la tráquea se divide en los bronquios izquierdo y derecho), o (3) hay 2 o más tumores en diferentes lóbulos del mismo pulmón.
El cáncer se ha propagado a los ganglios linfáticos por encima de la clavícula a ambos lados del cuerpo o a los ganglios linfáticos cercanos al otro pulmón, al otro lado del cuerpo del tumor principal (N3). No se ha propagado a otras partes del cuerpo (M0).
- (T3, N3, M0): El tumor es uno o más de los siguientes (T3): (1) tiene un tamaño de 5 a 7 cm, (2) ha crecido hacia la pared torácica, el revestimiento interno de la pared torácica (pleura parietal), el nervio frénico o el área alrededor del corazón (pericardio parietal), o (3) hay 2 o más tumores separados en el mismo lóbulo del pulmón.
- Estadio IVA
- (Cualquier T, Cualquier N, M1a): El tumor puede ser de cualquier tamaño y haber invadido la pleura, los bronquios, el mediastino u otras partes cercanas del cuerpo (Cualquier T). Puede haberse propagado a los ganglios linfáticos cercanos (Cualquier N). También puede (M1a): (1) haberse propagado al otro pulmón, (2) haberse propagado a la membrana que recubre los pulmones (pleura) o al pericardio (la membrana que recubre el corazón), o (3) haber causado la aparición de células cancerosas en el líquido que rodea el pulmón (derrame pleural maligno), o (4) haber causado la aparición de células cancerosas en el líquido que rodea el corazón (derrame pericárdico maligno).
- (Cualquier T, Cualquier N, M1b): El tumor puede ser de cualquier tamaño y haber invadido la pleura, los bronquios, el mediastino u otras partes cercanas del cuerpo (Cualquier T). Puede haberse propagado a los ganglios linfáticos cercanos (Cualquier N). El tumor también se ha propagado como un único tumor fuera del tórax. Podría tratarse de un ganglio linfático en otra parte del cuerpo o de un órgano como el cerebro, el hígado o el hueso (M1b).
- Estadio IVB
- (Cualquier T, Cualquier M, M1c): El tumor puede ser de cualquier tamaño y haber invadido la pleura, los bronquios, el mediastino u otras partes cercanas del cuerpo (Cualquier T). Puede haberse propagado a los ganglios linfáticos cercanos (Cualquier N). El tumor también se ha propagado a más de un tumor fuera del tórax. Este podría ser un ganglio linfático en otra parte del cuerpo, o el cerebro, el hígado o el hueso (M1c).
¿Cómo se trata el cáncer de pulmón de células no pequeñas?
El tratamiento del CPCNP depende del estadio del cáncer. Si fuma, deje de fumar lo antes posible. Fumar puede reducir la eficacia de sus tratamientos contra el cáncer y empeorar sus efectos secundarios.
Su tratamiento puede incluir algunos o todos los siguientes:
- Cirugía.
- Quimioterapia.
- Terapia dirigida.
- Inmunoterapia.
- Radioterapia.
- Tratamientos ablativos.
- Tratamiento paliativo.
- Ensayos clínicos.
Cirugía
La cirugía se puede utilizar en el tratamiento del CPCNP. El objetivo de la cirugía es extirpar la mayor cantidad posible de cáncer. Existen muchos procedimientos quirúrgicos diferentes para el tratamiento del CPCNP. Estos procedimientos incluyen:
- Resección en cuña: el cirujano extirpará una pequeña parte del pulmón afectado por el cáncer.
- Lobectomía: el cirujano extirpará el lóbulo del pulmón afectado por el cáncer.
- Neumonectomía: el cirujano extirpará todo el pulmón.
El tipo de cirugía que le puedan realizar dependerá de la ubicación y el tamaño del tumor, así como de su estado general de salud. También podrían hacerle pruebas de función pulmonar (PFP) antes de la cirugía para asegurarse de que la tolere.
También se puede recurrir a la cirugía si el cáncer se ha propagado (metástasis). Esto podría incluir la extirpación de tumores que se han propagado a partes del cuerpo como el cerebro, la columna vertebral o las glándulas suprarrenales.
Quimioterapia
La quimioterapia es el uso de medicamentos contra el cáncer que se administran por todo el cuerpo. Estos medicamentos pueden administrarse por vía intravenosa (IV) o por vía oral. La quimioterapia para el CPCNP puede combinarse con inmunoterapia o radioterapia. El tratamiento que reciba y su frecuencia dependerán del estadio del cáncer.
Los medicamentos utilizados para tratar el CPCNP incluyen: cisplatino, carboplatino, pemetrexed, paclitaxel, docetaxel, etopósido, gemcitabina, y vinorelbina. Su proveedor trabajará con usted para encontrar el mejor plan de quimioterapia para su cáncer y los posibles efectos secundarios de su tratamiento.
Terapia dirigida
Algunos cánceres tienen biomarcadores que ayudan a los profesionales de la salud a enfocar el tratamiento en ciertas mutaciones genéticas o receptores del tumor. Estos tratamientos se denominan terapias dirigidas. Se enfocan en esas mutaciones genéticas. Su médico analizará su tumor para detectar estos marcadores.
Las terapias dirigidas utilizadas en el tratamiento de mutaciones genéticas específicas incluyen:
- EGFR positivo: Amivantamab, afatinib, dacomitinib , erlotinib , gefitinib , lazertinib , y osimertinib .
- ALK positivo: Alectinib, brigatinib, ceritinib, crizotinib, ensartinib, y lorlatinib.
- Mutación KRAS G12C: Sotorasib y adagrasib.
- ROS1 positivo: Ceritinib, crizotinib, entrectinib, lorlatinib, y repotrectinib.
- BRAF V600E positivo: Dabrafenib con trametinib, encorafenib con binimetinib, y vemurafenib.
- Reordenamiento RET positivo: Cabozantinib, pralsetinib, y selpercatinib.
- Mutación de omisión del exón 14 del gen MET: Capmatinib , Crizotinib , y tepotinib .
- Mutaciones de ERBB (HER2): Ado-tratuzumab emtansina , fam-trantuzumab deructecan-nxki, y zenocutuzumab.
- Fusión genética NTRK positiva: Entrectinib, larotrectinib, y repotrectinib.
- Agentes antiangiogénicos/ Inhibidores del VEGF: Bevacizumab y ramucirumab.
Su proveedor le informará sobre la posibilidad de usar terapia dirigida para tratar su cáncer y los posibles efectos secundarios. Se están estudiando otros medicamentos de terapia dirigida en ensayos clínicos.
Inmunoterapia
Los medicamentos de inmunoterapia trabajan con el sistema inmunitario para destruir las células cancerosas. Los medicamentos de inmunoterapia que pueden usarse en el tratamiento del CPCNP son nivolumab, ipilimumab, cemiplimab, tremelimumab, pembrolizumab, atezolizumab, y durvalumab. Su proveedor le informará si estos medicamentos le ayudarán a tratar su cáncer y qué efectos secundarios podría tener. Se están estudiando otros medicamentos de inmunoterapia en ensayos clínicos.
Radioterapia
La radioterapia consiste en el uso de rayos X de alta energía para destruir células cancerosas. En el caso del CPCNP, la radiación puede utilizarse antes de la cirugía para reducir el tamaño del tumor y facilitar su extirpación. También puede utilizarse simultáneamente con quimioterapia, terapia dirigida o inmunoterapia. La radiación torácica también puede utilizarse para prevenir la reaparición del cáncer.
En ocasiones, el cáncer de pulmón se propaga a otras partes del cuerpo (metástasis). La radioterapia puede utilizarse para tratar la propagación del cáncer de pulmón a estas zonas, así como para aliviar el dolor causado por la propagación del cáncer.
Tratamiento ablativo
- Ablación por radiofrecuencia (ARF) se utiliza para tratar algunos tipos de tumores con una aguja y calor. La aguja caliente destruye las células cancerosas. Es posible que se caliente más de un tumor durante el procedimiento.
- Crioablación utiliza nitrógeno líquido o gas argón para congelar y matar las células cancerosas.
- Ablación por microondas utiliza microondas que penetran en el tumor a través de una sonda. El calor destruye las células cancerosas.
Tratamiento paliativo
El tratamiento paliativo se utiliza para aliviar los síntomas causados por el cáncer. No lo cura. Existen muchas opciones de tratamiento paliativo, como quimioterapia, radioterapia, cirugía, colocación de stents, terapias láser y extracción del exceso de líquido alrededor del corazón o los pulmones. Consulte con su médico sobre las opciones para aliviar sus síntomas.
Ensayos clínicos
Es posible que le ofrezcan un ensayo clínico como parte de su plan de tratamiento. Para obtener más información sobre los ensayos clínicos actuales, visite servicio de emparejamiento de ensayos clínicos OncoLink .
Toma de decisiones sobre el tratamiento
Su equipo de atención se asegurará de que participe en la elección de su plan de tratamiento. Esto puede ser abrumador, ya que podrían ofrecerle varias opciones. Tómese el tiempo para reunirse con diferentes proveedores y analizar sus opciones y qué es lo mejor para usted. Esta es una decisión personal. Sus amigos y familiares pueden ayudarle a analizar las opciones y las ventajas y desventajas de cada una, pero no pueden tomar la decisión por usted. Debe sentirse cómodo con su decisión; esto le ayudará a avanzar. Si tiene alguna pregunta o inquietud, no dude en llamar a su equipo.