Fallopian Tube Cancer: Staging and Treatment
encontrar mi
What is cancer staging?
Staging is the process of learning how much cancer is in your body and where it is. Imaging tests like ultrasound, CT, and MRI, blood level of the tumor marker CA-125, and surgery with a biopsy may be done to help determine your stage. Your providers need to know about your cancer and your health so that they can plan the best treatment for you.
Staging looks at the size of the tumor, where it is, and if it has spread to other organs. Both the FIGO (International Federation of Gynecologists and Obstetricians) system and the “TNM system,” as described by the American Joint Committee on Cancer are used to stage fallopian tube cancer. The TNM system has three parts:
- T-describes the size/location/extent of the "primary" tumor in the fallopian tube.
- N-describes if the cancer has spread to the lymph nodes.
- M-describes if the cancer has spread to other organs (called metastases).
Your healthcare provider will use the results of the tests you had to determine your FIGO or TNM result and combine these to get a stage from 0 to IV.
How is fallopian tube cancer staged?
Fallopian tube cancer is staged the same way that ovarian cancer is staged. Both the FIGO and TNM system are used. It is based on:
- If the cancer has spread, and if so, how far.
- How much cancer is in your body.
The staging systems are very complex. Below is a summary. Talk to your provider about the stage of your cancer.
- AJCC and FIGO Stage I:
- Cancer is only in the fallopian tube(s). It has not spread to nearby lymph nodes or to distant sites.
- AJCC and FIGO Stage IA:
- Cancer is in one fallopian tube and only inside the tube. It is not on the outside of the tube or in any fluid or washings from the abdomen (belly) and pelvis. It has not spread to nearby lymph nodes or to distant sites.
- AJCC and FIGO Stage IB:
- Cancer is in both fallopian tubes but not on the outside of the tube or in any fluid or washings from the abdomen or pelvis. It has not spread to nearby lymph nodes or distant sites.
- AJCC and FIGO Stage IC:
- The cancer is in one or both fallopian tubes and any of the following:
- IC1: The tissue around the tumor broke during surgery which could lead to cells leaking into the abdomen and pelvis.
- IC2: Cancer is on the outer surface of one or both fallopian tubes or the capsule burst before surgery.
- IC3: Cancer cells are found in the fluid or washing from the abdomen and pelvis.
- It has not spread to nearby lymph nodes or distant sites.
- The cancer is in one or both fallopian tubes and any of the following:
- AJCC and FIGO Stage II:
- The cancer is in one or both fallopian tubes and has spread to other organs in the pelvis or there is primary peritoneal cancer. It has not spread to nearby lymph nodes or distant sites.
- AJCC and FIGO Stage IIA:
- The cancer has spread or invaded the uterus or ovaries. It has not spread to nearby lymph nodes or to distant sites.
- AJCC and FIGO Stage IIB:
- The cancer is on the outer surface of or has grown into other nearby pelvic organs such as the bladder, the sigmoid colon, or the rectum. It has not spread to nearby lymph nodes or to distant sites.
- AJCC and FIGO Stage IIIA1:
- The cancer is in one or both fallopian tubes or there is primary peritoneal cancer, and it may have spread to nearby pelvic organs. It has spread to the retroperitoneal lymph nodes but not distant sites.
- AJCC and FIGO Stage IIIA2:
- The cancer is in one or both fallopian tubes or there is primary peritoneal cancer, and it has spread or grown into other organs outside the pelvis. During surgery no cancer can be seen in the belly but tiny deposits of cancer are found in the lining of the abdomen when it is looked at in the lab. The cancer may or may not have spread to retroperitoneal lymph nodes, but not distant sites.
- AJCC and FIGO Stage IIIB:
- There is cancer in one or both fallopian tubes or there is primary peritoneal cancer, and it has spread to organs outside the pelvis. The surgeon can see the cancer, but it is no bigger than 2cm across. It may or may not have spread to the retroperitoneal lymph nodes but has not spread to the inside of the liver or spleen or distant sites.
- AJCC and FIGO Stage IIIC:
- The cancer is in one or both fallopian tubes and there is primary peritoneal cancer, and it has spread to organs outside the pelvis. The cancer is larger than 2 cm across and may be on the outside of the liver or spleen. It may or may not spread to the retroperitoneal lymph nodes but has not spread to the inside of the liver or spleen or distant sites.
- AJCC and FIGO Stage IVA:
- Cancer cells are found in the fluid around the lungs with no other cancer spread.
- AJCC and FIGO Stage IVB:
- The cancer has spread to the inside of the spleen or live, lymph nodes that are not in the retroperitoneal area, and/or to organs or tissues outside the peritoneal cavity.
Treatment for Fallopian Tube Cancer
Treatment for fallopian tube cancer depends on things like your stage of disease, medical history, current health, your goals for treatment, and other factors. The goal of the treatment of fallopian tube cancer is to get rid of the cancer with few side effects. The treatments used can include:
- Surgery.
- Radiation.
- Chemotherapy.
- Clinical Trials.
A gynecologic oncologist often treats this type of cancer. They will do your surgery and manage your chemotherapy treatments. This is different from most cancer care providers for other types of cancer.
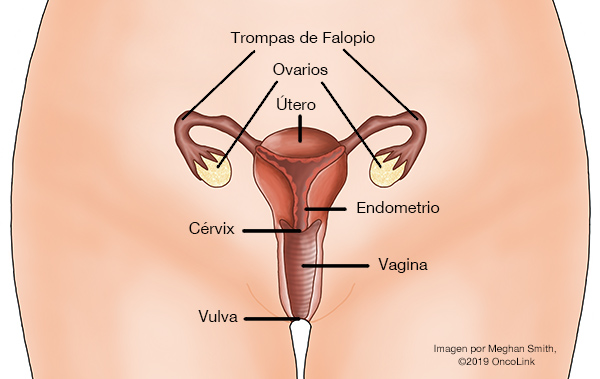
Surgery
The surgery type depends on the cancer stage seen in imaging tests. A salpingo-oophorectomy is used to treat early-stage fallopian tube cancer. It is the removal of either one or both fallopian tubes, and either one or both ovaries. In more advanced cancer stages, you may also need a total abdominal hysterectomy (removal of the uterus), bilateral salpingo-oophorectomy, infracolic omenectomy (removal of the abdominal lining), appendectomy (removal of the appendix), peritoneal washings, and peritoneal biopsies. Surgery may be used with radiation or chemotherapy, also called adjuvant therapy.
Radiation Therapy
Radiation therapy is the use of high-energy x-rays to kill cancer cells. Radiation is not a primary treatment for fallopian tube cancer. It is not very effective, and patients often have side effects. It may be used before surgery to help shrink the tumor.
Chemotherapy
Chemotherapy is the use of anti-cancer medications to kill cancer cells. Chemotherapy can be given after surgery to kill any leftover cancer cells. The most commonly used medications are cisplatin (platinum-based), carboplatin (platinum-based), gemcitabine, docetaxel, liposomal doxorubicin, cyclophosphamide, and paclitaxel.
In some cases, intraperitoneal chemotherapy will be used. This is when chemotherapy is injected directly into the abdomen and absorbed by nearby tissues and organs to kill cancer cells. Your provider will decide on a regimen that will best treat your cancer and your needs.
Targeted therapies can also be used to treat recurrent or advanced fallopian tube cancer. Targeted therapies target something specific to the cancer cells, which can help stop the cancer from growing. Bevacizumab, entrectinib, and larotrectinib are targeted therapies that may be used in fallopian tube cancer treatment. Neratinib, olaparib, and rucaparib are targeted therapies used in BRCA+ fallopian tube cancer.
Clinical Trials
You may be offered a clinical trial as part of your treatment plan. To find out more about current clinical trials, visit the OncoLink Clinical Trials Matching Service.
Making Treatment Decisions
Your care team will make sure you are included in choosing your treatment plan. This can be overwhelming as you may be given a few options to choose from. It feels like an emergency, but you can take a few weeks to meet with different providers and think about your options and what is best for you. This is a personal decision. Friends and family can help you talk through the options and the pros and cons of each, but they cannot make the decision for you. You need to be comfortable with your decision – this will help you move on to the next steps. If you ever have any questions or concerns, be sure to call your team.
You can learn more about fallopian tube cancer at OncoLink.org.