Module 10: Clinical Outcomes by Disease Site - The Use of Proton Therapy in the Treatment of Cancers of the Head and Neck
This content is no longer being maintained or updated. While it is available for review, please keep in mind the dates of creation, since some information may no longer be current.
For up-to-date proton therapy education designed for healthcare providers, please visit the Penn Radiation Medicine Institute. Current training and educational materials are available through our partnered and purchased programs.
encontrar mi
Introduction
Head and neck cancers constitute of variety of malignancies united by their anatomic complexity and close proximity to many critical structures governing vision, facial sensation, swallowing, saliva production, taste, smell, and speech. While many tumor subtypes can arise in the head and neck, the current module will focus on the mucosal squamous cell carcinomas and major salivary gland tumors. Skull base chordomas and chondrosarcomas are considered in a separate module.
Until recently, most published literature in proton therapy for head and neck squamous cell carcinoma focused on the treatment of nasal cavity and para-nasal sinus tumors. However, as we are starting to accumulate more clinical experience with proton therapy for head and neck cancer arising from other primary sites within the head and neck, we are starting to gain more insight into the value this modality may provide.
Intensity-modulated proton therapy for head and neck cancer
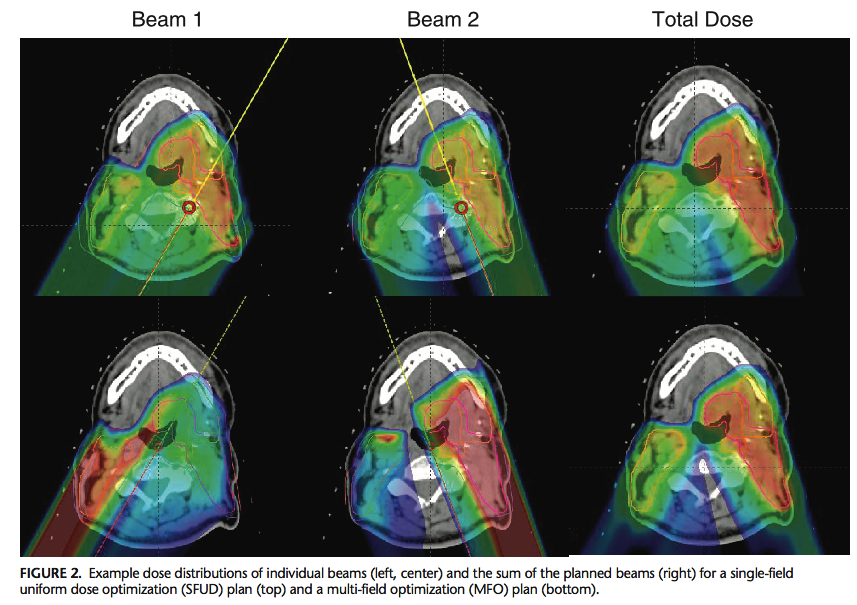
The development and implementation of intensity-modulated proton therapy (IMPT) represents a significant advance in proton radiation for head and neck cancer. Using this approach, multiple fields delivered with scanned beams deposit a non-uniform radiation dose over a target volume; the summation of all fields delivers the desired dose distribution. This technique is otherwise referred to as multi-field optimization (MFO). This approach contrasts with single field uniform dose (SFUD) optimization, in which two or three spot-scanned proton beams, each delivering a uniform dose, are used to cover the target while improving robustness and limiting dose to OARs. While IMPT has been shown to best spare organs at risk compared to SFUD, it is less robust to anatomic changes. This consideration becomes important in head and neck cancer when accounting for tumor response, weight loss on treatment, daily set up error, and dose uncertainty over a course of treatment, particularly in the definitive setting.
These concepts are illustrated in a dosimetric study of SFUD versus MFO planning in oropharyngeal squamous cell carcinoma from MD
Anderson. Investigators compared dose distributions in 3-field SFUD and MFO plans in 4 patients. Higher mean parotid doses (6.7 Gy), but better plan robustness, was observed in SFUD plans. While 2-field SFUD plans achieved better parotid-sparing compared to MFO, these plans were no longer more robust than MFO plans.
To better understand the effect of plan robustness, a second study simulated 10 IMPT plans on oropharyngeal cancer patients, generating 3700 variations of setup, range, and anatomical uncertainties. Investigators demonstrated failure to achieve prescription dose to the primary tumor in 31% of cases with considerable variation in doses to OARs due to uncertainties associated with IMPT. Adaptive re-planning, in which radiation treatment plans are modified during a course of treatment to account for anatomic changes, was able to compensate for these uncertainties, and therefore authors argue for the use of adaptive re-planning in this setting. However, the technical and logistic considerations of rapid adaptive re-planning are still an active area of investigation in radiation oncology clinics owing to the high cost and need for better patient selection in using this approach.
Clinical outcomes with proton radiation for oropharynx cancer
Recently, a number of studies have been published describing the potential clinical benefits of proton therapy in treating oropharyngeal cancer. Likely, the most substantive advantage to proton therapy in head and neck cancer will be its potential to reduce treatment morbidity. With this in mind, patient reported outcomes from 81 patients undergoing IMPT versus IMRT for definitive treatment of oropharyngeal cancer have been published using a prospective cohort of patients from MD Anderson Cancer Center. In this analysis, patient-reported changes in taste and appetite favored IMPT. Although no statistically significant differences in symptom burden were detected between modalities during the acute or chronic phases by top-11 symptom scoring, the overall burden of toxicity was reported to be higher in the IMRT cohort. Additionally, investigators at the University of Pennsylvania presented patient reported outcomes in 95 patients with oropharyngeal cancer treated with surgery and post-operative radiation using either VMAT or pencil beam scanning proton therapy. Protons versus VMAT were associated with improved rates of moderate-severe xerostomia (39% versus 65%, p = 0.08), which corresponding to more favorable dosimetry in saliva-producing structures. Further analysis indicated improved taste indices in patients treated with adjuvant, versus definitive radiation
Regarding survival outcomes, high level data are not yet mature to suggest that proton radiation in oropharyngeal cancer is superior to photon radiation. A retrospective case-matched analysis of 150 patients from MD Anderson Cancer Center treated with IMPT or IMRT demonstrated equivalent 3-year overall survival (94.3% versus 89.3%) and progression free survival (86.4% versus 85.8%) between the two modalities. This analysis also reported a statistically significant difference in the pre-planned composite endpoint of grade 3 weight loss or G-tube presence at 3 months and 1 year after treatment (OR=0.44; 95% CI: 0.19-1.0; p-value=0.05 and OR=0.23; 95% CI: 0.07-0.73; p-value=0.01, respectively). Outcomes from IMPT versus IMRT in oropharyngeal cancer patients are currently being compared prospectively in an ongoing Phase II/III trial at MD Anderson.
Proton therapy for other sites
As previously mentioned, a larger body of literature exists on the use of proton therapy for paranasal sinus and nasal cavity tumors, most of which consists of single arm single institutional experiences. Data from these studies have been pooled and analyzed in a meta-analysis consisting of 43 cohorts from 41 observational studies of patients with such cancers comparing charged particle therapy to photon radiation. Considering all patients treated with charged particle therapy, five year overall survival was significantly improved in the charged particle cohort compared to the photon cohort. A subgroup analysis comparing only proton therapy versus IMRT for these tumors demonstrated improved five year disease free survival (relative risk 1·44, 95% CI 1·01–2·05; p=0.045) and locoregional control (1·26, 1·05–1·51; p=0·011) in patients treated with protons. Though retrospective, these data at least suggest a benefit to proton therapy in this setting.
Tumors of the major salivary glands and well-lateralized skin cancers provide an opportunity to take advantage of the rapid dose fall off from proton radiation to spare OARs due to their unilateral presentation. In fact, conformal radiation with complete contralateral normal tissue sparing can be achieved when proton radiation is used to treat such sites with ipsilateral beams. This concept was studied in a retrospective analysis of 41 consecutive patients from Memorial Sloan Kettering Cancer Center, 23 of whom were treated with IMRT and 18 of whom were treated with proton therapy to ipsilateral sites only. IMRT significantly increased dose to spinal cord, brainstem , oral cavity, and contralateral parotid and submandibular glands compared to proton therapy. Physician reported acute dysgeusia, (5.6% vs. 65.2%, p<0.001), mucositis (16.7% vs. 52.2%, p=0.019), and nausea (11.1% vs. 56.5%, p=0.003) were also improved in patients treated with proton therapy relative to IMRT. These findings were attributed to the improved proton dosimetry.
Head and neck reirradiation
Re-irradiation has long been a recognized component of treatment for recurrent head and neck cancer for well-selected patients owing to relatively high rates of local recurrence,lack of effective salvage options, and potential for long-term survival even after local recurrence. As in other disease sites, reirradiation with proton therapy offers promise because of its ability to better spare integral dose to previously-irradiated tissue. The largest and most recently reported series of proton head and neck reirradiation was recently published out of Memorial Sloan Kettering Cancer Center. Their experience consisted of 92 consecutive patients followed for a median of 10.4 months and treated to a median dose of 60 Gy. 1 year overall survival was 65.2% and the toxicity profile was generally favorable with incidences of grade 3 mucositis, dysphagia, esophagitis, and dermatitis all less than 10%. There were 2 treatment-related deaths and 1 death from disease progression. These results suggest acceptable toxicity from head and neck reirradiation and survival outcomes and toxicity compare favorably with prior reports of head and neck photon reirradiation.
Conclusions
While we still are in the early stages of understanding technical aspects and clinical benefits of proton therapy for head and neck cancer, data thus far are encouraging. Future work will rely on wider utilization of IMPT through incorporation of adaptive re-planning and better assessing the impact of proton therapy on long term survival and quality of life in head and neck cancer patients.