Urethral Cancer
encontrar mi
Introduction
Carcinomas of the female urethra are rare diagnoses. Urethral cancer comprises approximately 0.02% of all cancers in women, with an average age at diagnosis of 60 years. Although the etiology is not clearly understood, the human papilloma virus ( HPV), especially type 16, may be associated with development of female urethral carcinoma.
Case History
History of Present Illness
The patient is a 72-year-old female who first noticed symptoms of decreasing urinary stream, dysuria, and progressively worsening hematuria several months ago. She saw her primary care physician at that time and was started on antibiotics, but did not get relief of her symptoms. Last month, she presented to the Emergency Department with symptoms of acute urinary retention. The emergency room physician experienced difficulty inserting a Foley catheter and thus a urologist was called for further management.
Past Medical History
Hypertension for twenty years, congestive heart failure, gout, and bilateral cataracts.
Past Surgical History
Total abdominal hysterectomy and bilateral salpingo-oopherectomy (TAH/BSO) for fibroids 1979.
Past Gynecological History
The patient states that she has never been pregnant. She underwent menarche at age 13 and menopause at age 52. She denies exogenous estrogen or oral contraceptive use in the past or present. She denies any history of positive Pap smears, but has not had one in the past 18 years. The patient also denies any history of venereal disease.
Medications and Allergies
Clonidine, Allopurinol, Lasix, and Coumadin.
Penicillin causes facial and body hives.
Social History
The patient is married and lives with her husband in a small apartment. She is a retired factory worker. The patient has a 50-pack-year history of cigarette smoking, but states that she quit 2 years ago. The patient also reports a history of drinking "a fifth" of hard liquor per week, but claims that she quit 5 months ago.
Family History
The patient recalls a paternal aunt with leukemia, diagnosed and treated at a young age. She also reports a paternal and maternal cousin with breast cancer, both of whom are deceased now. The patient is unsure of either the ages at diagnosis or the causes of death of these family members.
Review of Systems
The patient has noticed a ten-pound weight loss in the last six months. She also complains of some difficulty sleeping lately. Otherwise as per HPI.
Physical Examination
GENERAL: Patient is an obese, African-American female in no acute distress and who appears her stated age.
VITALS: Pulse 76, Respiratory Rate 16, Blood Pressure 140/80, Karnofsky Performance Scale score 70.
HEENT: Head is normocephalic, atraumatic, PERRLA, EOMI. Oral cavity and oropharynx reveal poor dentition with no lesions or masses.
CHEST: Lungs are clear to auscultation bilaterally. No crackles, rhonchi, or wheezes are noted and chest expansion is symmetrical.
CARDIOVASCULAR: Heart is regular rate and rhythm, with normal S1 and S2 and no S3 or S4. A grade II/VI early systolic murmur is heard best at the left sternal border. No rubs or gallops are noted. Peripheral pulses are present and equal bilaterally.
ABDOMEN: Soft, non-tender, non-distended, with positive bowel sounds. No masses or organomegaly are noted.
GU: Urethral meatus is erythematous, with a 3 x 4 cm induration of the anterior vaginal wall palpated immediately posterior to the urethra. No tumor visible at the urethral opening. Unable to pass a small speculum past the introitus secondary to patient discomfort.
EXTREMITIES: No clubbing, cyanosis, or edema appreciated.
MUSCULOSKELETAL: Motor strength 5/5 bilaterally, upper and lower extremities.
NEURO: Patient is alert and oriented to person, place, and time. Cranial nerves II-XII intact bilaterally. Good finger to nose movements bilaterally.
Data
LABS: CBC, serum chemistry panel and urinalysis are all within normal limits.
IMAGING/DIAGNOSTIC STUDIES: A cystoscopy is performed and reveals an irregularly-shaped mass extending from the urethral meatus, along the entire length of the urethra with involvement of the bladder neck. A transurethral resection of both the proximal and distal areas is subsequently performed to allow for free flow of urine.
Pathology of the resected specimen reveals a well- to moderately-differentiated adenocarcinoma. Retrograde pyelograms are also performed and are within normal limits.
A CT scan of the abdomen and pelvis shows no abnormal lymph nodes. Bone scan reveals only arthritic changes of the bilateral knees, ankles, and thoracic spine. Chest x-ray shows no evidence of metastasis.
Assessment and Plan
The patient is a 72-year old African-American female with a T3N0M0, stage II adenocarcinoma of the entire length of the urethra.
The patient is status-post a transurethral debulking procedure for relief of acute urinary retention. Postoperatively, she is doing very well and currently denies any dysuria or hematuria.
After a discussion with her multi-modality team, she declines any further surgical options.
The patient is recommended to undergo external beam radiotherapy with concurrent chemotherapy consisting of 5-FU and Cisplatin. She would receive whole pelvic radiation, with a possible prescription of 5040 cGy of photons over 5 weeks, for example. This would then need to be followed by an interstitial implant for continued antitumor effects.
The patient is explained the benefits and the risks, including stricture, incontinence and fistula, of radiation therapy as well as the alternatives to treatment. After discussion with her husband, the patient agrees to proceed with external beam radiation and concurrent chemotherapy. She will consider a possible SYED interstitial implant upon conclusion of this treatment plan.
Discussion
Natural History
Urethral meatus tumors at an early stage may resemble a urethral caruncle or as a prolapse of the mucosa. Lesions tend to enlarge and ulcerate as they progress. Later stage tumors can extend upward into the bladder or downward into the vaginal mucosa.
Clinical Presentation and Natural History
The most common presenting sign is bleeding. About 30% of patients present with:
- pain
- difficulty in urination
- frequent micturition
- urinary retention or overflow incontinence
Early stage urethral tumors may present as a papillary growth within the urethra or as a ulcerative lesion. They may resemble a urethral caruncle or even appear as a prolapse of the mucosa. Lesions tend to enlarge and ulcerate as they progress. Spread from the primary lesion is by local extension and infiltration in an upward and/or downward direction, with subsequent involvement of the bladder neck or vaginal mucosa and vulva, respectively.
Lymphatic drainage is an important anatomical factor in urethral cancers. Advanced urethral tumors (stage II and III) have pelvic or inguinal lymph node involvement in about 35-50% of cases. The most common sites of metastasis are lung, liver, bone, and brain.
Diagnostic Workup
- H&P, including detailed pelvic examination under anesthesia.
- Urethroscopy
- Cystoscopy
- Punch biopsy
- Urine cytology
- CT scan of abdomen and pelvis
TNM Classification
Primary tumor (T) (men and women) | |
Tx | Primary tumor cannot be assessed |
T0 | No evidence of primary tumor |
Ta | Noninvasive papillary, polypoid, or verrucous carcinoma |
Tis | Carcinoma in situ |
T1 | Tumor invades subepithelial connective tissue |
T2 | Tumor invades any of the following: corpus spongiosum, prostate, periurethral muscle |
T3 | Tumor invades any of the following: corpus cavernosum, beyond prostate capsule, anterior vagina, bladder neck |
T4 | Tumor invades other adjacent organs |
Regional lymph nodes (N) | |
Nx | Regional lymph nodes cannot be assessed |
N0 | No regional lymph node metastasis |
N1 | Metastasis in a single lymph node, 2 cm or less in greatest dimension |
N2 | Metastasis in a single lymph node, more than 2 cm in greatest dimension, or in multiple lymph nodes |
Distant metastasis (M) | |
Mx | Distant metastasis cannot be assessed |
M0 | No distant metastasis |
M1 | Distant metastasis |
Pathologic Classification
Histology
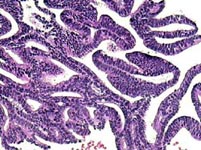
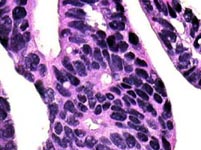
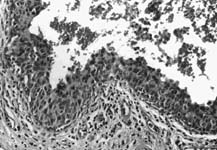
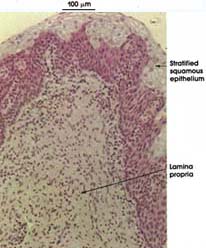
[4]
Low-power microscopic view (H & E stain) | High-power microscopic view (H & E stain) |
Normal squamous epithelium | Carcinoma in situ |
Prognostic Factors
Given that urethral cancers in women are so rare and often have a very poor prognosis, there is little consensus on their treatment. Grigsby and his associates determined that the most significant factors affecting prognosis in females with urethral cancer are tumor size and histology [5].
Distal Urethral Cancer Treatment Options
Distal tumors tend to be low stage and cure rates of 70-90% have been reported with either local excision or radiation therapy [6]. If positive inguinal nodes, add ipsilateral nodal dissection or irradiation.
Proximal Urethral Cancer Treatment Options
These cases are often associated with invasion of the bladder and a high incidence of pelvic lymph node metastasis. They are usually treated with radiotherapy for organ preservation. Very large lesions are treated with combinations of surgery, radiotherapy, and chemotherapy [5].
Radiation Therapy Techniques
Small tumors of the meatus can be treated with an interstitial implant. Interstitial brachytherapy using iridium-192 afterloading implants may be used up to a total dose of 60-70 Gy (0.4 Gy/hour) in 6-7 days.
Large, extensive tumors often require a combination of external-beam irradiation and an implant. The whole pelvis is treated to a dose of 50 Gy with a 10-15 Gy boost if the inguinal lymph nodes are positive. The addition of the interstitial implant brings the total dose to 70-80 Gy [1]. Gupta and researchers studied the treatment outcomes in locally advanced urethral cancers using Iridium-192 transperineal interstitial brachytherapy. They reported actuarial data with 5-year local control rates of 52%, disease specific survival of 53%, and overall survival of 38% [7].
Conclusions
The lack of consensus on the treatment of women with urethral cancer is due to the rarity of the tumor and the poor prognosis of women with large lesions. Tumor size and histology appear to be the most significant clinical factors. Brachytherapy is a viable treatment option for many of these patients.