Gallbladder Cancer: Staging and Treatment
What is staging for cancer?
Staging is the process of learning how much cancer is in your body and where it is. For gallbladder cancer, blood tests like metabolic chemistry, liver function tests, and tumor marker levels (CEA and CA 19-9), and other tests like ultrasound, cholangiography, CT, MRI, and/or PET scans may be used to help stage your cancer. Your providers need to know about your cancer and your health so that they can plan the best treatment for you.
Staging looks at the size of the tumor where it is, and if it has spread to other organs. The staging system for gallbladder cancer is called the “TNM system,” as described by the American Joint Committee on Cancer. It has three parts:
- T-describes the size/location/extent of the "primary" tumor in the gallbladder.
- N-describes if the cancer has spread to the lymph nodes.
- M-describes if the cancer has spread to other organs (metastases).
Your healthcare provider will use the results of the tests you had to find your TNM result and combine these to get a stage from 0 to IV.
How is gallbladder cancer staged?
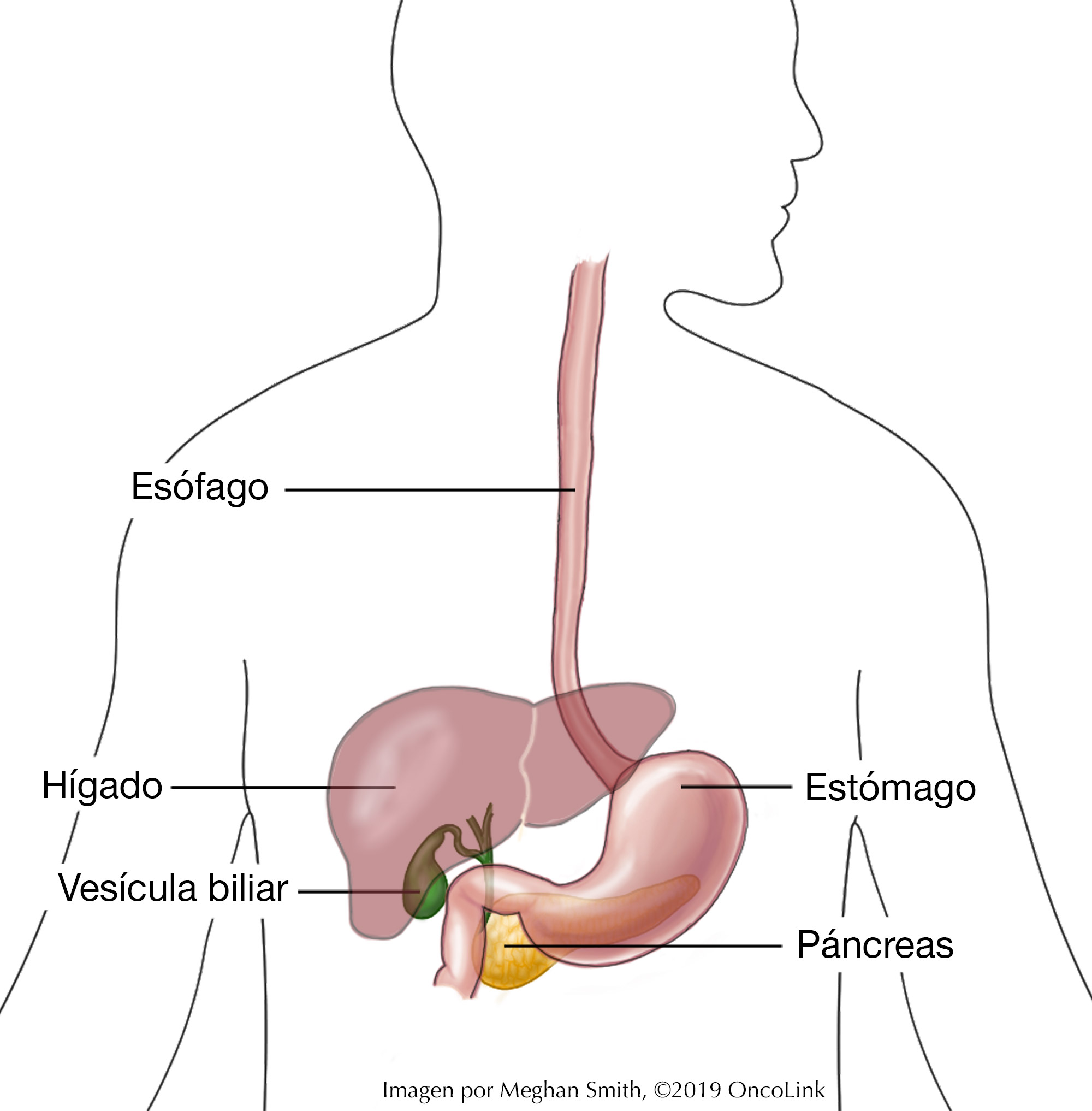
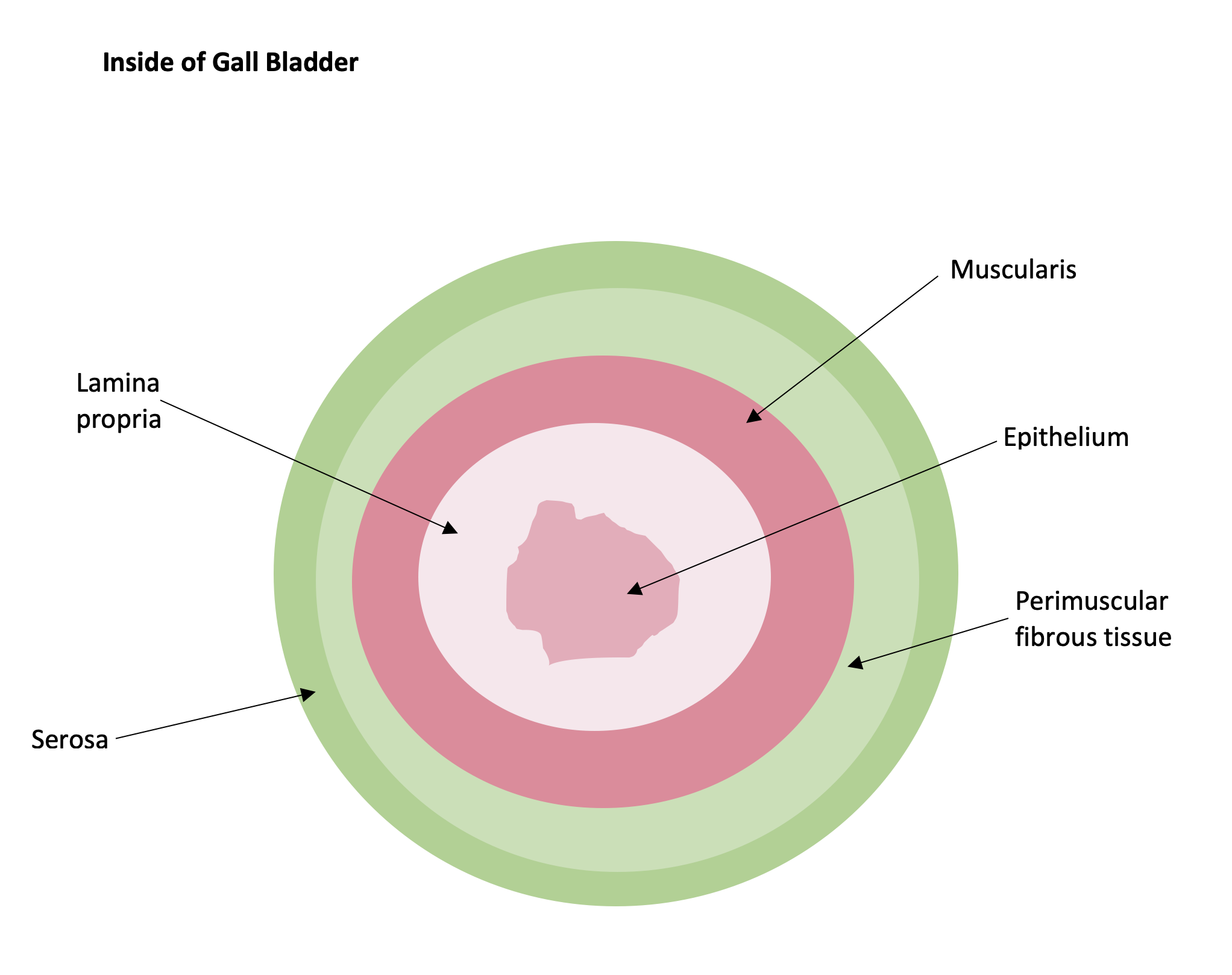
Most gallbladder cancers start on the inside wall of the gallbladder. This is called the epithelium. The tumor can grow toward other parts of the gallbladder and may take up all or some of the space in the gallbladder.
Staging for gallbladder cancer is based on:
- The location, size of the tumor, and if it has grown through the wall of the gallbladder to nearby organs.
- If the tumor has spread to the lymph nodes and the number of lymph nodes affected.
- If the tumor has spread to other organs. This is called metastasis.
The gallbladder is made of many layers, how deep the tumor grows from the inside layer (epithelium) to the outer layers (lamina propria, musclaris, perimuscular fibrous tissue, and serosa) is important in the staging.
Staging helps to guide your treatment options. The staging system is very complex and below is a summary. Talk to your provider about the stage of your cancer.
- Stage 0: The tumor is only in the inner layer of the gallbladder and has not grown into any other layers of the gallbladder. The tumor has not spread to lymph nodes or other organs.
- Stage I: The tumor has grown into more layers of the gallbladder like the lamina propria or the muscularis (muscle layer). The tumor has not spread to lymph nodes or other organs.
- Stage II (A or B): The tumor has spread through the muscularis. It may have also spread in the tissue lining the abdominal cavity (the peritoneum) or the tissue on the side of the liver (but has not spread to the liver). The tumor has not spread to lymph nodes or other organs.
- Stage III (A or B): The tumor has grown through the outer layer of the gallbladder (serosa). The tumor may have grown into the liver or another part of the body like the stomach, small intestine, colon, bile ducts, or pancreas. The tumor has not grown into the veins/arteries that go into the liver. The tumor may have also grown into the lymph nodes but no more than three lymph nodes are involved. It has not spread to other organs beyond the stomach, small intestine, colon, bile ducts, or pancreas.
- Stage IV (A or B): The tumor has grown into the veins/arteries that go into the liver or 2 organs outside of the liver. The tumor has spread to the lymph nodes and other organs.
Your provider may also use the grade of your cancer when planning your treatment. The grade tells more about what the tumor cells look like under the microscope. The grade can be 1-3. Higher-grade tumors may grow faster.
How is gallbladder cancer treated?
Treatment for gallbladder cancer is based on the size and location of the tumor and if it has spread to the lymph nodes or other organs. There can be more than one type of treatment used to treat gallbladder cancer. Some of the treatments used for gallbladder cancer are:
- Surgery.
- Radiation.
- Chemotherapy.
- Palliative Therapy.
Surgery
If the cancer can be taken out by surgery, it is called resectable. If not, it is unresectable. If the tumor is early stage and only in the inner layer of the gallbladder, the whole gallbladder can be removed. This is called a cholecystectomy. Once the tumor has grown into the muscle, parts of the liver may also need to be removed. If the tumor is larger, a lobe of the liver may need to be removed. This is called hepatectomy/lobectomy. Sometimes a procedure known as a Whipple (pancreaticduodenectomy) is used in later-stage gallbladder tumors.
There are also palliative procedures where the goal is not to remove the cancer but to relieve symptoms. This could include relieving a blockage of the bile duct (biliary stent). Stage IV tumors are not often treated with surgery.
Radiation
Radiation is the use of high-energy X-rays to kill cancer cells. Radiation can be used after surgery or to relieve symptoms. It can also be used for people who have a late-stage tumor or if they are not healthy enough for surgery. Radiation may be used with or without chemotherapy. Radiation usually targets the tumor (or tumor bed (where the tumor was), if post-surgery) and the lymph nodes in that area.
Chemotherapy
Chemotherapy is the use of anti-cancer medicines that go through your whole body. These medicines may be given through a vein IV (intravenously) or by mouth.
Chemotherapy is used to treat gallbladder cancer either after surgery (adjuvant therapy) or as the only type of treatment. It can also be used to relieve symptoms. This is called palliative therapy. The chemotherapy medications used to treat gall bladder cancer are 5-FU, cisplatin, capecitabine, oxaliplatin, gemcitabine, and albumin-bound paclitaxel. These medications may be used alone or in combination.
Targeted therapies target specific genetic or molecular markers on tumors. Some gallbladder tumors have these markers. Your team may test a sample of your tumor for them. Targeted medications used in the treatment of some gallbladder cancers are entrectinib, larotrectinib, pembrolizumab, and dostarlimab-gxly.
Palliative Therapy
Palliative therapy is used to relieve symptoms that are caused by the tumor. They do not cure the cancer. Symptoms like pain, nausea, and jaundice can be treated with palliative therapy. A biliary stent or catheter can be placed to treat jaundice. This will help the bile drain out of the bile ducts. A surgical biliary bypass is another palliative procedure that can be used in some patients to allow bile to flow more freely.
Clinical Trials
You may be offered a clinical trial as part of your treatment plan. To find out more about current clinical trials, visit the Oncolink Clinical Trials Matching Service.
Making Treatment Decisions
Your care team will make sure you are included in choosing your treatment plan. This can be overwhelming as you may be given a few options to choose from. It feels like an emergency, but you can take a few weeks to meet with different providers and think about your options and what is best for you. This is a personal decision. Friends and family can help you talk through the options and the pros and cons of each, but they cannot make the decision for you. You need to be comfortable with your decision – this will help you move on to the next steps. If you ever have any questions or concerns, be sure to call your team.
Referencias
American Cancer Society. Gallbladder Cancer.
American Cancer Society. (2018). Gallbladder Cancer Stages.
American Cancer Society (2018). Signs and Symptoms of Gallbladder Cancer.
American Cancer Society (2018). Tests for Gallbladder Cancer.
Azizi, A. A., Lamarca, A., McNamara, M. G., & Valle, J. W. (2021). Chemotherapy for advanced gallbladder cancer (GBC): A systematic review and meta-analysis. Critical reviews in oncology/hematology, 163, 103328.
Cai, J., Xu, L., Cai, Z., Wang, J., Zhou, B., & Hu, H. (2015). MicroRNA-146b-5p inhibits the growth of gallbladder carcinoma by targeting epidermal growth factor receptor. Molecular Medicine Reports, 12(1), 1549-1555.
Cancer.net (2023). Gallbladder Cancer: Types and Treatment.
Cariati, A., Piromalli, E., & Cetta, F. (2014). Gallbladder cancers: associated conditions, histological types, prognosis, and prevention. European Journal of Gastroenterology & Hepatology, 26(5), 562-569.
Cavallaro, A., Piccolo, G., Panebianco, V., Lo Menzo, E., Berretta, M., Zanghì, A., ... & Cappellani, A. (2012). Incidental gallbladder cancer during laparoscopic cholecystectomy: managing an unexpected finding. World J Gastroenterol, 18(30), 4019-4027.
De Lorenzo, S., Garajova, I., Stefanini, B., & Tovoli, F. (2021). Targeted therapies for gallbladder cancer: An overview of agents in preclinical and clinical development. Expert opinion on investigational drugs, 30(7), 759-772.
Hundal, R., & Shaffer, E. A. (2014). Gallbladder cancer: epidemiology and outcome. Clinical Epidemiology, 6, 99-109.
Liebe, R., Milkiewicz, P., Krawczyk, M., Bonfrate, L., Portincasa, P., & Krawczyk, M. (2015). Modifiable Factors and Genetic Predisposition Associated with Gallbladder Cancer. A Concise Review. J Gastrointestin Liver Dis, 24(3), 339-348.
Martel, G., & Auer, R. C. (2016). Resection of Gallbladder Cancer, Including Surgical Staging. In Atlas of Upper Gastrointestinal and Hepato-Pancreato-Biliary Surgery (pp. 599-609). Springer Berlin Heidelberg.
Matos, C., Santiago, I., Maciel, J., & Levy, A. D. (2015). Gallbladder Neoplasms. Gastrointestinal Imaging,474.
National Comprehensive Cancer Network. NCCN Guidelines Version 2.2023, Hepatocellular Carcinoma.
National Comprehensive Cancer Network. NCCN Guidelines Version 3.2023, Biliary Tract Cancers.
Qadan, M. & Kingham, T. P. (2016). Technical Aspects of Gallbladder Cancer Surgery. Surgical Clinics of North America, 96(2), 229-245.
Sasaki, T., Hiroki, K., & Yamashita, Y. (2013). The role of epidermal growth factor receptor in cancer metastasis and microenvironment. BioMed Research International, article ID 546318, 8 pages, 2013. doi:10.1155/2013/546318
Sicklick, J. K., Fanta, P. T., Shimabukuro, K., & Kurzrock, R. (2016). Genomics of gallbladder cancer: the case for biomarker-driven clinical trial design. Cancer and Metastasis Reviews, 1-13.
Stinton, L. M., & Shaffer, E. A. (2012). Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver, 6(2), 172-187.
Wernberg, J. A., & Lucarelli, D. D. (2014). Gallbladder cancer. Surgical Clinics of North America, 94(2), 343-360.